Acinetobacter baumannii in Lebanon
Authors: Rayane Rafei and Monzer Hamze
Laboratoire Microbiologie Santé et Environnement (LMSE), Doctoral School of Science & Technology, Faculty of Public Health, Lebanese University, Tripoli, Lebanon (rayanerafei@hotmail.com; mhamze@monzerhamze.com)
Reviewer: Ziad Daoud
College of Medicine, Central Michigan University, Mount Pleasant, MI, United States (zdaoud@mihealthclinic.com)
Hospital epidemiology of Acinetobacter baumannii in Lebanon
Although A. baumannii appears to be endemic in the Lebanese clinical settings with the description of many outbreaks, its true burden is still not adequately captured despite the increasing number of publications in the last few years (Dandachi et al., 2019). For instance, A. baumannii was the most predominant pathogen of ventilator-associated pneumonia among adult ICU patients between 2008 and 2017 at a Lebanese tertiary referral center (Kanafani et al., 2019). It was also responsible for 4% of all recorded bacterial bloodstream infections over 10 years among patients with hematological malignancies (Haddad et al., 2021). It was also the third pathogen isolated after Staphylococcus aureus and Pseudomonas aeruginosa among patients admitted to a Burn care center between 2014 and 2018 (Bourgi et al., 2020). The majority of the Lebanese isolates were multi-drug resistant with high percentages of carbapenem-resistant A. baumannii (CRAB) varying between 60% and 100% (Nawfal Dagher et al., 2019; Chamoun et al., 2016; Rafei et al., 2015; Dahdouh et al., 2016; Al Atrouni et al., 2016; Hammoudi et al., 2015; Hajjar Soudeiha et al., 2018; Moghnieh et al., 2019). Even with the increasing trend of CRAB, many hopeful interventions such as carbapenem sparing regimens and appropriate infection prevention and control measures showed success in containing the outbreaks and reducing CRAB (Chamieh et al., 2019; Osman et al., 2020; Chamieh et al., 2021; Rizk et al., 2022; Moussally et al., 2021; Moghnieh et al., 2020).
OXA-58 was the unique carbapenemase described in the earliest epidemiological studies (published in or before 2011) and was harbored by the global clones 1 (sequence type 20 “ST20”IP, a single locus variant of ST1IP), 2 (ST2IP), and 3 (ST3IP) (Zarrilli et al., 2008; Di Popolo et al., 2011). In global clone 1 strains incriminated in an outbreak that occurred between 2004 and 2005 in a university hospital in Beirut, blaOXA-58 was carried by a pABIR plasmid and bounded by 2 insertion sequences (IS18 and ISAba3) explaining thus its dissemination (Zarrilli et al., 2008). However, in agreement with worldwide observations, a marked shift from OXA-58 to OXA-23 was witnessed in the following studies with ST2IP (a main ST in the global clone 2) being the main OXA-23 producing clone (Nawfal Dagher et al., 2019; Rafei et al., 2015; Dahdouh et al., 2016; Al Atrouni et al., 2016; Hajjar Soudeiha et al., 2018; Osman et al., 2020; Rafei et al., 2014). Despite the predominance of OXA-23-producing ST2 strains, other mechanisms and clones were also detected but to a lesser degree. Isolates belonging to ST636IP and carrying blaOXA-72 (blaOXA-24 variant) on pMAL-1 plasmid were responsible for a nosocomial outbreak along with other ST2IP and ST2-likeIP carrying blaOXA-23 on Tn2006 (Makke et al., 2020). NDM-1, produced by ST85IP strains, was firstly detected in Syrian refugees and then in Lebanese patients (Al Atrouni et al., 2016; Rafei et al., 2014). Other STs positive for blaNDM-1 were also identified as ST25IP and ST708IP (Rafei et al., 2015; Al Atrouni et al., 2016). In another multi-regional study, the beta-lactamase gene blaGES-11 was associated with blaOXA-23 isolates in 90% of CRAB collected in 2012 (Hammoudi et al., 2015). Generally, the genomic context of resistance genes was sparingly addressed in Lebanon. In one of the sequenced blaNDM-1 carrying ST85IP isolates, blaNDM-1 along with 14 copies of the aphA6 amikacin resistance genes were enclosed within a novel transposon Tn7 named Tn6924 (Mann et al., 2022). In another ST2IP strain, each of the four blaOXA-23 copies was located in an AbaR4 copy, and blaTEM and aphA1 genes were present in a novel variant of AbGRI2 known as AbGRI2-15 (Liepa et al., 2022).
IP: sequence types (ST) defined according to the MLST scheme of the Pasteur Institute.
Extra-hospital epidemiology of Acinetobacter baumannii in Lebanon
Nationwide and regional studies investigating the extra hospital epidemiology of A. baumannii in Lebanon, isolated it from several environmental (soil, water, sewage), animal (pets, livestock), and food (milk, vegetables, meat, cheese) samples (Rafei et al., 2015; Al Atrouni et al., 2016; Al Bayssari et al., 2015). These isolates were generally susceptible to the tested antimicrobial agents including beta-lactams and non-beta-lactam antibiotics (Rafei et al., 2015; Al Atrouni et al., 2016). However, some isolates from the livestock and poultry animals (horse, cattle, pig, and fowl) showed resistance to carbapenems and harbored enzymes like the blaOXA-23, blaOXA-58, and blaOXA-143 (Rafei et al., 2015; Al Bayssari et al., 2015).
Concerning clonality, they were so diverse belonging to different STs, generally, novel ones, which were different from the STs found among hospital isolates. However, some identified STs are common in health care settings as ST1IP, ST2IP, and ST10IP (Rafei et al., 2015; Al Atrouni et al., 2016; Al Bayssari et al., 2015). Studying two susceptible environmental isolates belonging to global clone 1 helped to better redraw the population structure of this clone, which now encompasses 2 major clades including 5 main antibiotic-resistant lineages and 4 single-isolate antibiotic-susceptible lineages outside of the 2 clades (Koong et al., 2021).
IP: sequence types (ST) defined according to the MLST scheme of the Pasteur Institute.
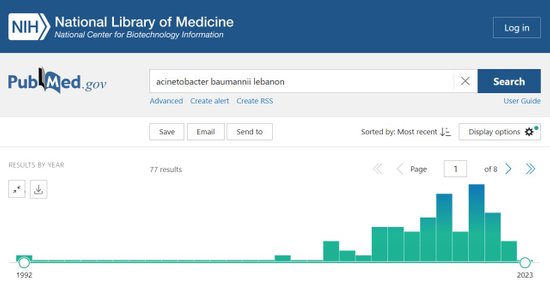
Screenshot of the PubMed website while searching for articles on Acinetobacter baumannii in Lebanon as of 30.01.2023
(https://pubmed.ncbi.nlm.nih.gov/?term=acinetobacter+baumannii+lebanon&timeline=expanded&sort=date)
References
Dandachi I, Azar E, Hamouch R, Maliha P, Abdallah S, Kanaan E, Badawi R, Khairallah T, Matar GM, Daoud Z. Acinetobacter spp in a third world country with socio-economic and immigrants challenges. J Infect Dev Ctries. 2019 Nov 30;13(11):948-955.
doi: 10.3855/jidc.11341
PMID: 32087065
Kanafani ZA, El Zakhem A, Zahreddine N, Ahmadieh R, Kanj SS. Ten-year surveillance study of ventilator-associated pneumonia at a tertiary care center in Lebanon. J Infect Public Health. 2019 Jul-Aug;12(4):492-495.
doi: 10.1016/j.jiph.2019.01.057
PMID: 30737129
Haddad S, Jabbour JF, Hindy JR, Makki M, Sabbagh A, Nayfeh M, Boustany M, El-Zein S, Tamim H, Zakhem AE, El Cheikh J, Bazarbachi A, Kanj SS. Bacterial bloodstream infections and patterns of resistance in patients with haematological malignancies at a tertiary centre in Lebanon over 10 years. J Glob Antimicrob Resist. 2021 Dec;27:228-235.
doi: 10.1016/j.jgar.2021.09.008
PMID: 34607062
Bourgi J, Said JM, Yaakoub C, Atallah B, Al Akkary N, Sleiman Z, Ghanimé G. Bacterial infection profile and predictors among patients admitted to a burn care center: A retrospective study. Burns. 2020 Dec;46(8):1968-1976.
doi: 10.1016/j.burns.2020.05.004
PMID: 32522390
Nawfal Dagher T, Al-Bayssari C, Chabou S, Antar N, Diene SM, Azar E, Rolain JM. Investigation of multidrug-resistant ST2 Acinetobacter baumannii isolated from Saint George hospital in Lebanon. BMC Microbiol. 2019 Feb 2;19(1):29.
doi: 10.1186/s12866-019-1401-2
PMID: 30710998
Chamoun K, Farah M, Araj G, Daoud Z, Moghnieh R, Salameh P, Saade D, Mokhbat J, Abboud E, Hamze M, Abboud E, Jisr T, Haddad A, Feghali R, Azar N, El-Zaatari M, Chedid M, Haddad C, Zouain Dib Nehme M, Barakat A, Husni R; Lebanese Society of Infectious Diseases Study Group (LSID study group). Surveillance of antimicrobial resistance in Lebanese hospitals: retrospective nationwide compiled data. Int J Infect Dis. 2016 May;46:64-70.
doi: 10.1016/j.ijid.2016.03.010
PMID: 26996458
Rafei R, Pailhoriès H, Hamze M, Eveillard M, Mallat H, Dabboussi F, Joly-Guillou ML, Kempf M. Molecular epidemiology of Acinetobacter baumannii in different hospitals in Tripoli, Lebanon using blaOXA-51-like sequence based typing. BMC Microbiol. 2015 May 16;15:103.
doi: 10.1186/s12866-015-0441-5
PMID: 25976451
Dahdouh E, Hajjar M, Suarez M, Daoud Z. Acinetobacter baumannii isolated from Lebanese patients: Phenotypes and genotypes of resistance, clonality, and determinants of pathogenicity. Front Cell Infect Microbiol. 2016 Nov 25;6:163.
PMID: 27933276
Al Atrouni A, Hamze M, Jisr T, Lemarié C, Eveillard M, Joly-Guillou ML, Kempf M. Wide spread of OXA-23-producing carbapenem-resistant Acinetobacter baumannii belonging to clonal complex II in different hospitals in Lebanon. Int J Infect Dis. 2016 Nov;52:29-36.
doi: 10.1016/j.ijid.2016.09.017
PMID: 27663910
Hammoudi D, Moubareck CA, Hakime N, Houmani M, Barakat A, Najjar Z, Suleiman M, Fayad N, Sarraf R, Sarkis DK. Spread of imipenem-resistant Acinetobacter baumannii co-expressing OXA-23 and GES-11 carbapenemases in Lebanon. Int J Infect Dis. 2015 Jul;36:56-61.
doi: 10.1016/j.ijid.2015.05.015
PMID: 26004171
Hajjar Soudeiha M, Dahdouh E, Daoud Z, Sarkis DK. Phenotypic and genotypic detection of β-lactamases in Acinetobacter spp. isolates recovered from Lebanese patients over a 1-year period. J Glob Antimicrob Resist. 2018 Mar;12:107-112.
doi: 10.1016/j.jgar.2017.09.016
PMID: 28986323
Moghnieh R, Araj GF, Awad L, Daoud Z, Mokhbat JE, Jisr T, Abdallah D, Azar N, Irani-Hakimeh N, Balkis MM, Youssef M, Karayakoupoglou G, Hamze M, Matar M, Atoui R, Abboud E, Feghali R, Yared N, Husni R. A compilation of antimicrobial susceptibility data from a network of 13 Lebanese hospitals reflecting the national situation during 2015-2016. Antimicrob Resist Infect Control. 2019 Feb 20;8:41.
doi: 10.1186/s13756-019-0487-5
PMID: 30828445
Chamieh A, Nawfal TD, Ballouz T, Afif C, Juvelekian G, Hlais S, Rolain JM, Azar E. Control and elimination of extensively drug-resistant Acinetobacter baumanii in an intensive care unit. Emerg Infect Dis. 2019 Oct;25(10):1928-1931.
PMID: 31538925
Osman M, B Halimeh F, Rafei R, Mallat H, Tom JE, Raad EB, M Diene S, Jamal S, Atrouni AA, Dabboussi F, Moudani W, Madec JY, Saras E, Lupo A, Haenni M, Rolain JM, Hamze M. Investigation of an XDR-Acinetobacter baumannii ST2 outbreak in an intensive care unit of a Lebanese tertiary care hospital. Future Microbiol. 2020 Oct;15:1535-1542.
PMID: 33215520
Chamieh A, Zgheib R, El-Sawalhi S, Yammine L, El-Hajj G, Zmerli O, Afif C, Rolain JM, Azar E. Trends of multidrug-resistant pathogens, difficult to treat bloodstream infections, and antimicrobial consumption at a tertiary care center in Lebanon from 2015-2020: COVID-19 Aftermath. Antibiotics (Basel). 2021 Aug 21;10(8):1016.
doi: 10.3390/antibiotics10081016
PMID: 34439065
Rizk NA, Zahreddine N, Haddad N, Ahmadieh R, Hannun A, Bou Harb S, Haddad SF, Zeenny RM, Kanj SS. The impact of antimicrobial stewardship and infection control interventions on Acinetobacter baumannii resistance rates in the ICU of a tertiary care center in Lebanon. Antibiotics (Basel). 2022 Jul 7;11(7):911.
doi: 10.3390/antibiotics11070911
PMID: 35884165
Moussally M, Zahreddine N, Kazma J, Ahmadieh R, Kan SS, Kanafan ZA. Prevalence of antibiotic-resistant organisms among hospitalized patients at a tertiary care center in Lebanon, 2010-2018. J Infect Public Health. 2021 Jan;14(1):12-16.
doi: 10.1016/j.jiph.2020.11.006
PMID: 33341479
Moghnieh R, Tamim H, Jadayel M, Abdallah D, Al-Kassem R, Kadiri H, Hafez H, Al-Hassan S, Ajjour L, Lakkis R, Jisr T, Samaha NL, Haddad N. The effect of temporary closure and enhanced terminal disinfection using aerosolized hydrogen peroxide of an open-bay intensive care unit on the acquisition of extensively drug-resistant Acinetobacter baumannii. Antimicrob Resist Infect Control. 2020 Jul 14;9(1):108.
doi: 10.1186/s13756-020-00772-z
PMID: 32665037
Zarrilli R, Vitale D, Di Popolo A, Bagattini M, Daoud Z, Khan AU, Afif C, Triassi M. A plasmid-borne blaOXA-58 gene confers imipenem resistance to Acinetobacter baumannii isolates from a Lebanese hospital. Antimicrob Agents Chemother. 2008 Nov;52(11):4115-20.
doi: 10.1128/AAC.00366-08
PMID: 18725447
Di Popolo A, Giannouli M, Triassi M, Brisse S, Zarrilli R. Molecular epidemiological investigation of multidrug-resistant Acinetobacter baumannii strains in four Mediterranean countries with a multilocus sequence typing scheme. Clin Microbiol Infect. 2011 Feb;17(2):197-201.
doi: 10.1111/j.1469-0691.2010.03254.x
PMID: 20456455
Rafei R, Dabboussi F, Hamze M, Eveillard M, Lemarié C, Gaultier MP, Mallat H, Moghnieh R, Husni-Samaha R, Joly-Guillou ML, Kempf M. Molecular analysis of Acinetobacter baumannii strains isolated in Lebanon using four different typing methods. PLoS One. 2014 Dec 26;9(12):e115969.
doi: 10.1371/journal.pone.0115969
PMID: 25541711
Makke G, Bitar I, Salloum T, Panossian B, Alousi S, Arabaghian H, Medvecky M, Hrabak J, Merheb-Ghoussoub S, Tokajian S. Whole-genome-sequence-based characterization of extensively drug-resistant Acinetobacter baumannii hospital outbreak. mSphere. 2020 Jan 15;5(1):e00934-19.
PMID: 31941816
Rafei R, Dabboussi F, Hamze M, Eveillard M, Lemarié C, Mallat H, Rolain JM, Joly-Guillou ML, Kempf M. First report of blaNDM-1-producing Acinetobacter baumannii isolated in Lebanon from civilians wounded during the Syrian war. Int J Infect Dis. 2014 Apr;21:21-3.
doi: 10.1016/j.ijid.2014.01.004
PMID: 24560830
Mann R, Rafei R, Gunawan C, Harmer CJ, Hamidian M. Variants of Tn6924, a novel Tn7 family transposon carrying the blaNDM metallo-β-Lactamase and 14 copies of the aphA6 amikacin resistance genes found in Acinetobacter baumannii. Microbiol Spectr. 2022 Feb 23;10(1):e0174521.
doi: 10.1128/spectrum.01745-21
PMID: 35019774
Liepa R, Mann R, Osman M, Hamze M, Gunawan C, Hamidian M. Cl415, a carbapenem-resistant Acinetobacter baumannii isolate containing four AbaR4 and a new variant of AbGRI2, represents a novel global clone 2 strain. J Antimicrob Chemother. 2022 Feb 2;77(2):345-350.
doi: 10.1093/jac/dkab399
PMID: 34741594
Rafei R, Hamze M, Pailhoriès H, Eveillard M, Marsollier L, Joly-Guillou ML, Dabboussi F, Kempf M. Extrahuman epidemiology of Acinetobacter baumannii in Lebanon. Appl Environ Microbiol. 2015 Apr;81(7):2359-67.
doi: 10.1128/AEM.03824-14
PMID: 25616788
Al Atrouni A, Hamze M, Rafei R, Eveillard M, Joly-Guillou ML, Kempf M. Diversity of Acinetobacter species isolated from different environments in Lebanon: a nationwide study. Future Microbiol. 2016 Sep;11:1147-56.
PMID: 27545979
Erratum in: Future Microbiol (PMID: 27883288)
Al Bayssari C, Dabboussi F, Hamze M, Rolain JM. Emergence of carbapenemase-producing Pseudomonas aeruginosa and Acinetobacter baumannii in livestock animals in Lebanon. J Antimicrob Chemother. 2015 Mar;70(3):950-1.
doi: 10.1093/jac/dku469
PMID: 25406297
Koong J, Johnson C, Rafei R, Hamze M, Myers GSA, Kenyon JJ, Lopatkin AJ, Hamidian M. Phylogenomics of two ST1 antibiotic-susceptible non-clinical Acinetobacter baumannii strains reveals multiple lineages and complex evolutionary history in global clone 1. Microb Genom. 2021 Dec;7(12):000705.
PMID: 34874246